PainRelief.com Interview with:
- Brinda Krish, D.O., lead author of the study and an anesthesiology resident at Detroit Medical Center.
- Padmavathi Patel, M.D., principal investigator of the study and Medical Director, Northstar Anesthesia at John D. Dingell Veteran Hospital.
PainRelief.com: What is the background for this study? What are the main findings?
Dr. Padmavathi Patel: Pain is a major contributor to health care costs and a common cause of long-term disability (about $61.2 billion/year) in lost productivity due to pain.
76.2 million Americans (one in four) have suffered from pain that lasts longer than 24 hours (2013).
Numerous literature such as:
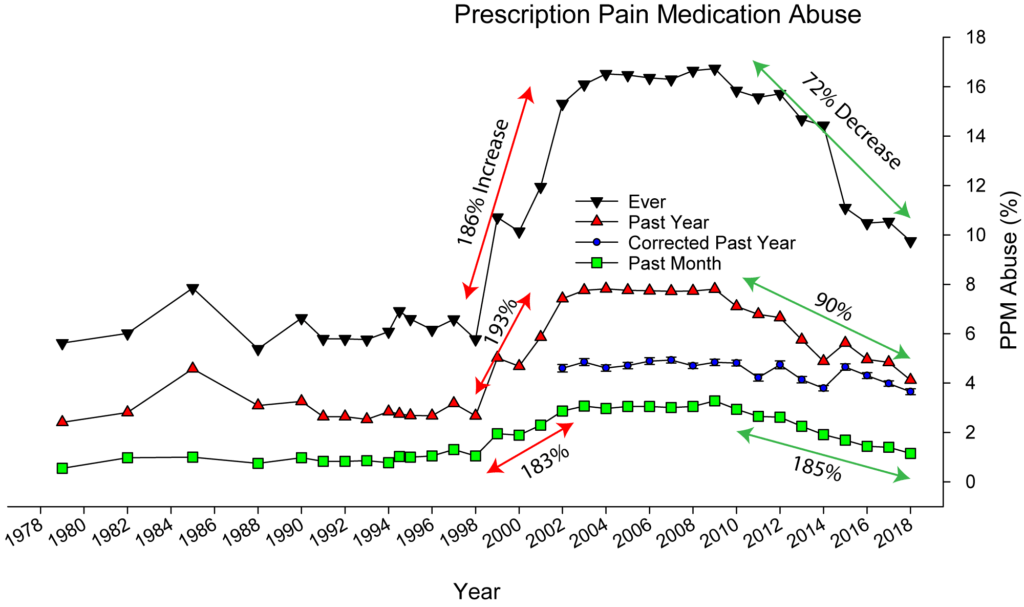
1. “Use of prescription opioids in the treatment of pain has increased notably over recent decades.”
2. “Rates of death from prescribed opioids increased four fold between 2000 and 2014.”
3. “16,651 opioid related deaths in 2010.”
4. “The problem of opioid overuse and dependence is seen in the military as well as in civilian.”
-Opioid-related side effects could lead to a delay in recovery.
-Pain control is more challenging for military population.
-More extensive injuries and greater pain severity is seen in survivors of combat- related blast injuries compared to those of non-blast civilians and also they require larger opioid doses.
-Pain is a very common patient complaint, both in veteran and non-veteran populations.
-Among the 5.7 million unique patients seen annually with in the Department of Veterans Affairs (DVA), more than half of these patients experience chronic pain.
In 2017, The DVA and the United States Department of Defense (DoD) published an updated guidelines on opioid therapy for chronic pain that strongly recommends against initiation of long-term opioid use and recommends alternatives, including non-pharmacologic therapy, such as Acupuncture, which has been shown to be effective for treating a variety of painful conditions.
Acupuncture techniques have been in existence for centuries, with roots tied to Eastern Asia. Traditional acupuncture involves the insertion of very thin needles at specific trigger points around the body to relieve pain. Battlefield acupuncture (BFA), developed by a U.S. Air Force doctor uses needles that are inserted at various trigger points in the ear. In 2013, $5.4 million was awarded to the Departments of Defense and Veterans Affairs to teach BFA to healthcare providers in both the military and the Department of Veterans Affairs and assess it. In light of the opioid epidemic, there is a strong need to decrease perioperative opioid use. Opioid use due to postoperative pain along with perioperative anxiety has been linked to increased length of hospital stay, increased morbidity and mortality, and ultimately higher healthcare costs.
Battlefield acupuncture was introduced into Veterans Health Administration (VHA) in the last few years and in VHA, clinicians of various disciplines (MDs, DOs, PAs, nurse-practitioners), can currently obtain clinical privilege to provide it.
I received the Battlefield acupuncture training at John D. Dingell VA medical Center, Detroit and I was surprised with the outcomes of chronic pain patients. As an anesthesiologist I know pain after the surgery is common, often severe and largely unnecessary. I discussed these concerns with the surgeons and created the protocol to use BFA for general surgical patients and traditional acupuncture for hip replacement patients as an adjuvant to the standard protocol for acute post-surgical pain control.
Effective relief of postoperative pain is vital. Such pain probably prolongs hospital stay, as it can affect all the organ systems with side effects. Post op pain remains grossly under treated, with up to 70% of patients reporting moderate to severe pain following surgery.
Multimodal pain control not only can result in earlier discharge from hospital, but it may also reduce the onset of chronic pain syndromes.
2 studies performed TA (n=21), Controls given sham acupuncture (n=21). BFA (n=28), Controls given sham acupuncture (n=36). Measured variables included post-operative opioid requirements, postoperative pain, the incidence of PONV, and patient satisfaction scores
Key conclusions use of Battlefield acupuncture and Traditional acupuncture reduced post-operative opioid requirements, post-operative pain scores (pain intensity) and increased patient satisfaction scores. BFA also reduced PONV in patients.