PainRelief.com Interview with:
Mario Moric M.S.
Department of Anesthesiology
Rush University Medical
Center Department of Anesthesiology
PainRelief.com: What is the background for this study? What are the main findings?
- Prescription Pain Medicine (PPM) abuse has become a national problem and is now consider an epidemic. In 2012, health care providers wrote 259 million prescriptions for opioid pain medication; enough for every American adult to have a bottle of opioids.
- With the recent public information campaign about the epidemic and the possible addictive nature of opioid prescription pain medications, the abuse rates have declined. We examined data from the National Survey on Drug Use and Health (NSDUH) public data derived from a national survey.
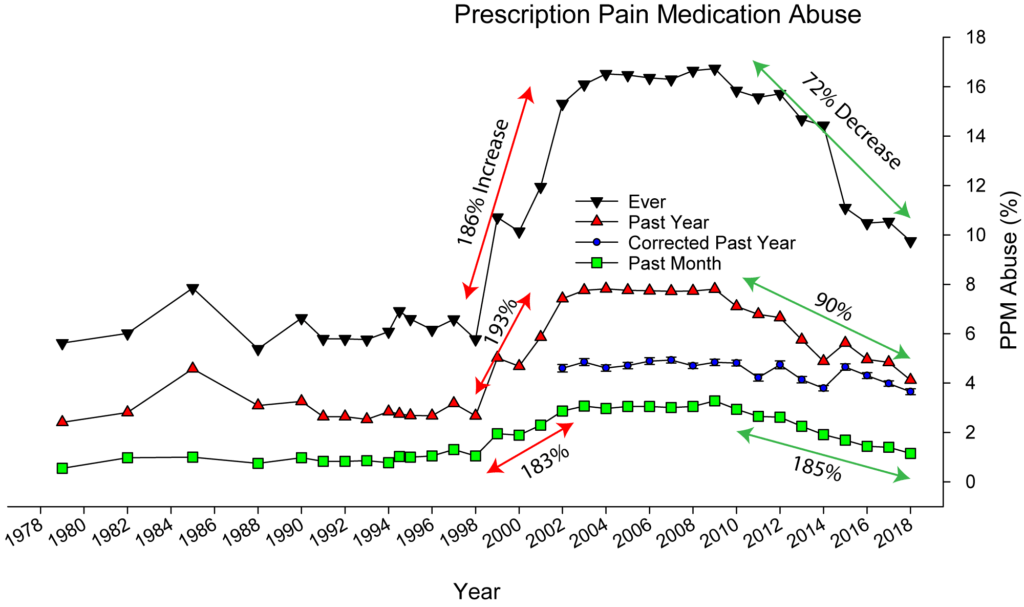
- We have raw data (actual reported rates of PPM abuse, see attached image) and weighted data (corrected for the sampling design). Looking at the raw data you can see that abuse rates for lifetime use (highest line), past year use (middle red line) and past month use (bottom green line) are all more or less stable until 1998 after which we saw huge increase. From 1998 to 2004 the lifetime use increased 186%, the past year use increased 193% and the past month use increased 183%. Then the decrease, from 2009 to 2018 the lifetime use decreased 72%, the past year use decreased 90% and the past month use decreased 185%.
- Using the weighted data, the past year use decreases 26% and was statistically significant, indicating a real world decrease in prescription pain medication abuse.